Welcoming a new life into the world is a remarkable journey filled with anticipation, challenges, and profound joy. From the intensity of labor and delivery to the delicate postpartum period, every step is a unique experience that shapes both the mother and baby’s well-being. Understanding these stages is essential for ensuring a safe and healthy transition for both.
The postpartum phase, often referred to as the "fourth trimester," is a critical time for recovery and adjustment. Mothers experience significant physical and emotional changes that require care and attention. Proper postpartum support not only aids in healing but also strengthens the bond with the newborn, setting the foundation for long-term health and happiness.
By focusing on comprehensive care during labor, delivery, and the postpartum period, families can navigate this transformative time with confidence and resilience. It's a journey of care, connection, and growth for both mother and child.
labor & delivery
Labor involves the process of the cervix dilating and thinning due to uterine contractions, preparing for childbirth. According to the National Institute of Child Health and Human Development, labor encompasses different stages: early labor, active labor, and the pushing phase, which leads to delivery. This process can vary widely in duration and intensity for each person.
Delivery can occur through vaginal birth or cesarean section (C-section). In vaginal deliveries, the baby and placenta exit through the vagina. In C-sections, the baby and placenta are delivered surgically through an incision in the abdomen. Each method has distinct recovery protocols depending on factors like labor complexity or medical conditions.
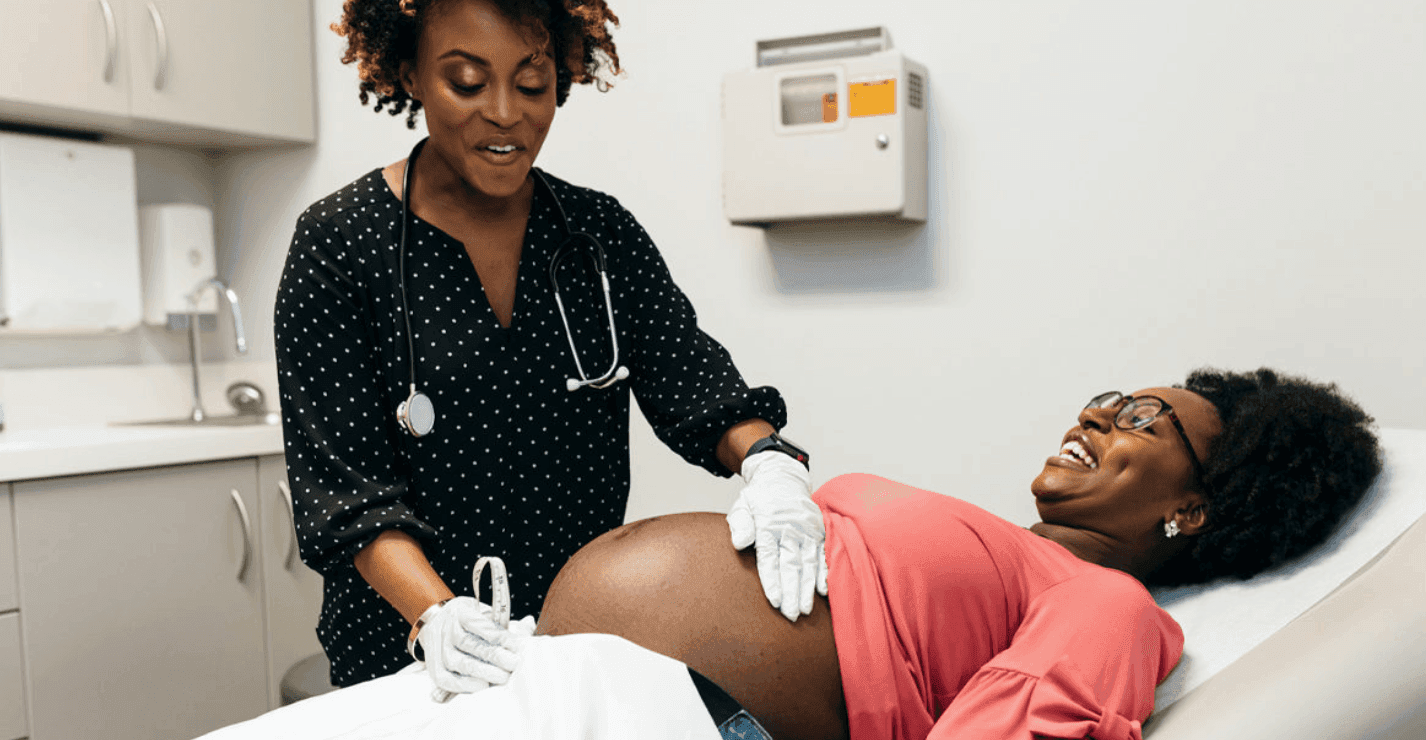
Healthcare teams monitor closely during labor using tools to assess the baby’s vital signs and the progress of contractions. Pain management options, including epidurals or non-pharmacological techniques like breathing exercises, are offered to ensure comfort. A collaborative approach respects individual birth plans while addressing any medical needs that may arise.
Efforts during labor and delivery focus on safely welcoming the newborn while supporting the physical and emotional well-being of the mother.
giving birth natural
Natural childbirth refers to delivering a baby without medical interventions such as epidurals or other pain-relief medications. This approach focuses on using the body’s innate ability to give birth, emphasizing techniques like breathing exercises, movement, and relaxation to manage pain and progress labor.
Women opting for natural birth often prepare by attending childbirth education classes, working with doulas, or practicing specific methods like Lamaze or hypnobirthing. These techniques help reduce fear and anxiety during labor, promoting a calm and focused environment.
During labor, healthcare providers support natural births by encouraging position changes, utilizing water therapy, and providing quiet, supportive spaces. They closely monitor both the baby’s and mother’s health to ensure safety throughout the process. Labor companions, such as partners or family members, often play a vital role by offering physical and emotional comfort.
Natural births are typically associated with shorter recovery times, as they avoid potential side effects of medical interventions. However, healthcare professionals remain vigilant to transition to medical assistance if complications arise, ensuring the well-being of both mother and baby.
What does postpartum mean?
Postpartum, or postnatal, refers to the period immediately after childbirth, typically lasting six to eight weeks, although some changes can extend beyond this timeframe. This phase marks a critical time for a mother’s physical recovery and emotional adjustment, as well as bonding with her newborn.
What are the three stages of postpartum?
Healthcare providers classify postpartum into three distinct phases based on the timeline of recovery and potential medical concerns:
Acute Phase: Occurs during the first six to 12 hours after childbirth. Mothers are closely monitored for complications such as postpartum hemorrhage, eclampsia, and swelling. Healthcare teams check vital signs like blood pressure and heart rate.
Subacute Phase: Spanning from 24 hours to six weeks postpartum, this phase involves significant physical recovery and hormonal adjustments. Common issues during this time include postpartum depression, urinary incontinence, and cardiomyopathy.
Delayed Phase: Ranges from six weeks to six months postpartum. Gradual physical and emotional recovery continues in this phase, with muscles, tissues, and energy levels returning to their pre-pregnancy state.
Postpartum recovery timeline
The recovery period after childbirth varies by individual, but certain general timelines can offer insight into what mothers might experience:
First 6-12 hours: Intense monitoring for complications. Healing in areas like the perineum begins.
**First 6 weeks: **Active physical recovery, including the uterus shrinking (uterus involution) and hormone stabilization.
**Up to 6 months: **Gradual resolution of remaining symptoms, such as fatigue or body aches. Emotional and mental stability improves, although challenges like breastfeeding concerns or mood changes may persist.
Physical symptoms
Common physical symptoms mothers experience postpartum include:
Soreness and pain: Especially in the perineum, resulting from vaginal delivery or tearing. Ice packs and warm water rinses are simple remedies.
Vaginal discharge (lochia): Bleeding and spotting that shift from red to light brown over six weeks. Tampons are not recommended; sanitary pads are preferred.
Uterus involution: The uterus reduces to its pre-pregnancy size over several weeks, accompanied by mild cramping.
Emotional symptoms
Emotional changes occur as the body adjusts hormonally:
**Baby blues: **Temporary feelings of sadness and tearfulness, usually resolving within two weeks.
**Postpartum depression: **Persistent and intense sadness, requiring medical treatment through therapy or medication.
**Postpartum anxiety: **Excessive worry and physical symptoms like insomnia or heart palpitations. Often linked to hormonal changes, it can co-occur with depression.
When should I contact my healthcare provider?
Mothers should reach out to their healthcare provider if they notice symptoms suggesting complications:
Heavy bleeding or large blood clots beyond six weeks.
Severe abdominal or pelvic pain.
Signs of infection like fever, chills, or foul-smelling discharge.
Persistent feelings of sadness, hopelessness, or thoughts of harm to self or the baby.
Physical symptoms such as chest pain, shortness of breath, or leg swelling, which could indicate conditions like deep vein thrombosis (DVT).
Postpartum checkups are pivotal for addressing concerns and ensuring the mother’s recovery remains on track.
What to expect during postpartum recovery
Postpartum recovery involves significant physical and emotional adjustments. The body begins healing from childbirth while adapting to care for a newborn. This period extends beyond the first six to eight weeks, with some symptoms lasting several months.
Physical recovery
Physical changes can include soreness in the perineal area, especially after vaginal delivery. Perineal swelling, bruising, or tears may cause lingering discomfort. Pain relief measures include sitting on a cushion, applying cold packs, or using perineal bottles for hygiene.
Vaginal discharge, known as lochia, starts with heavy bleeding but reduces over time. Bleeding changes from bright red to pinkish-brown and eventually fades to a light discharge over several weeks. Uterus involution, the process of the uterus returning to pre-pregnancy size, often causes cramping during the first few days postpartum.
Breastfeeding mothers may experience breast engorgement, tender nipples, or milk flow issues as their breasts adjust to feeding a baby. Non-breastfeeding mothers may feel discomfort until milk production ceases. Hormonal fluctuations could trigger sweating, hair loss, or acne.
Emotional recovery
Hormonal changes combined with lack of sleep may lead to mood swings or irritability. About 70%-80% of mothers experience "baby blues" in the first two weeks. If sadness or anxiety becomes overwhelming or persists, it may indicate postpartum depression, requiring medical attention.
Common challenges
Women often deal with fatigue, disrupted sleeping patterns, and the demands of caring for a newborn. Changes in appetite, diminished sexual desire, and urinary incontinence are also common. Breastfeeding struggles, such as latch issues or low milk supply, may add stress.
Tips for recovery
Prioritizing rest, proper nutrition, and hydration accelerates healing. Gentle postpartum exercises, such as pelvic floor strengthening, support physical recovery. Regular healthcare check-ins help monitor progress and address concerns like severe pain or infections. Seeking help for mental health challenges or caregiving tasks reduces stress and ensures a smoother transition into motherhood.
Care
Navigating labor, delivery, and the postpartum period requires patience, support, and self-care. Every experience is unique, and understanding the physical and emotional demands of this journey helps foster confidence in new parents.
Prioritizing rest, nutrition, and professional guidance ensures a healthier recovery while strengthening the bond between mother and baby. With the right care and resources, families can embrace this transformative time with resilience and joy.